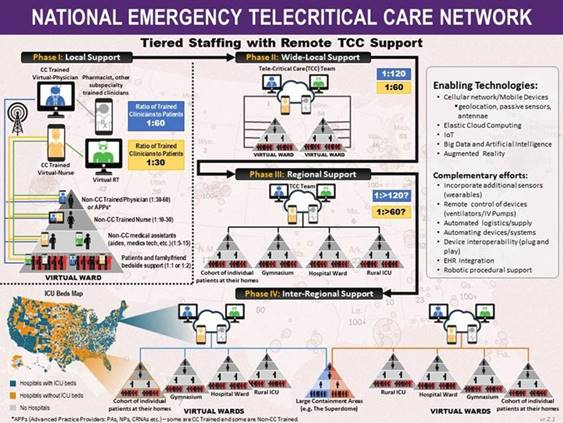
The U.S. Army’s Telemedicine and Advanced Technology Research Center (TATRC) has issued a Request for Project Proposals (RPP) to support the rapid development, deployment and testing of the National Emergency Telecritical Care Network (NETCCN) – a cloud-based, low-resource, stand-alone health information management system for the creation and coordination of flexible and extendable “virtual critical care wards.” These high acuity, virtual wards would bring high-quality critical care capability to nearly every bedside, be it healthcare facility, field hospital, or gymnasium.
PROGRAM BACKGROUND:
This program is specifically focused on preparation for COVID-19 related critical care capability shortages. Although the United States has more critical care beds per capita than other developed nations, emerging national and international experience with COVID-19-related critical illness suggests a high level of oncoming system stress on critical care resources and a likely potential for intensive care unit (ICU) beds and care teams to be overwhelmed.
Tele-critical care can be a powerful force-multiplier in the extension of limited critical care resources in both high-census urban centers and rural communities in which access to critical care – facilities, equipment and trained clinicians – is limited even under normal conditions. Many local and regional health systems have invested extensively in telemedicine capabilities, but many of these systems lack sufficient scalability, are limited both in interoperability with other telehealth systems and scope and reach of partner provider-networks and supported tele-clinical services.
The vision for this program is to extend local tele-critical care capability sets to a broader, flexible network – first locally, then step-wise regionally and nationally – that can be leveraged wherever there is need.
SOLUTION REQUIREMENTS:
This RPP focuses on enhanced development of integrated technologies and clinical workflows to establish and rapidly scale virtual wards. The program will support the extension of high-quality intensive care to traditional (e.g. critical access hospitals and clinics) and non-traditional and temporary healthcare facilities (e.g. field hospitals and gymnasiums) which lack adequate critical care expertise and resources necessary for care of COVID-19-related illnesses. Enhanced white papers should specifically address providing EXISTING technologies available for other use cases that can be rapidly adapted to establishing a National Emergency Tele Critical Care Network (NETCCN). Existing technologies which should be included are as follows:
- Mobile communications capabilities including synchronous audio/video, asynchronous messaging, and access to continuous monitoring
- Clinician-facing web portal and/or mobile-based application (goal is availability on every device)
- Capability for basic documentation in real-time as well as data collection and reporting
- Cloud-based information storage including ability for later offloading via PDF or HL7
Specific requirements for the creation of these “virtual wards” (i.e., cohorts of patients that are managed together and with continuity by the tele critical care [TCC] teams) include the following:
- Self-contained health information management system (or system of systems) using elastic cloud computing at a minimum, IoT connections, and anticipated incorporation of future AI to enable:
- Patient flow management
- Patient level information management
- Continuity of care through shift change, provider turnover, and patient transfer using lightweight patient hand-off tools.
- Integrated audio-visual communications capability
- Information sharing and reporting capabilities:
- A governance structure or “network of networks” must be implemented to coordinate this response
- Reporting and data visualization tools of both patient and system level data are crucial for information sharing, dissemination of consensus best-practice recommendations, measures of system stress, and rapid reallocation of resources.
- Survey capabilities – of patients/caregivers, local clinicians, and remote TCC experts should – should be included.
- Patient-level data should be aggregated and stored for later analysis, can eventually be batch loaded into existing EMRs when resources allow
- System should allow for alerts, bulletins, and other timely communications to be pushed out to users
- Integrated information sharing
- Coverage/staffing/care team model(s) for virtual wards to include tiered staffing concepts with local proceduralists (as available) supported by the technology solution developed in this proposal and serviced by tele critical care clinicians.
- The system will need to include a method to verify credentials of tele critical care clinicians/teams who participate as service providers.
SCOPE OF WORK:
The goals of this RPP are to provide a first system for deployment within 45 days of award (end of Task 3), a refined system for deployment within 6 months of award (end of Task 4), and a final system for deployment within 18 months of award (end of Task 5).
*Refer to the full RPP for details related to each task.
*Optimal Applicant Teams: It is preferred that proposed projects address the entire scope of work. An optimal team responding to this RPP would consist of clinical experts, technology experts, computer scientists, and entities with experience in change management and rapid cycle innovation. However, enhanced white paper submissions that only partially address the requirement are also encouraged, with the understanding that these Offerors may be teamed with other Offerors with complementary expertise to construct a complete team that can address the full scope of work.
Task 1: Initial system configuration and alpha testing (t = 15 days)
Offerors are expected to bring forth systems which they have currently developed that would facilitate the capture, exchange and archiving of medical clinical information as described above. This phase is largely based on the validation and initial outfitting of systems that would support minimal consultation services from the virtual wards to tele critical care teams including asynchronous and synchronous communications from/to the appropriate team member (including the patient/bedside caregiver when appropriate) and self-contained documentation of care and orders tools. The Offeror must also describe the primary use case(s) for the product and the care team/staffing model/care model for intended use. The Offeror must also be able to describe information assurance and cyber security features of their product.
Task 2: Rapid Development and beta testing (t = 30 days)
After initial alpha testing to validate system capabilities as claimed by Offerors, the selected systems will be moved into the second phase of prototyping and testing. Additional minimum features include patient regulating and team coordination functions and database storage functions. The Offeror must also describe additional use cases and alternate care team models for their product. Field testing with local/small cohorts of actual users is expected.
Task 3: Reliability Testing, Deployment and Enhancement (t = 45 days)
During this phase, the systems must be fielded to actual users and experience real world use for a large cohort (at least a regional geographic area) of patients. Simultaneously, new adaptations can be made to fit the specifics of the COVID-19 pandemic, so movement from generic data transmission to more specific formats and clinical practices that represent COVID-19 support. A plan/program for “just-in-time” training for anticipated users (ideally a part of the application) should be included.
Task 4: Automated Improvements (t = 3-6 months)
This task aims to incorporate automated improvements that can enhance the care as well as reduce time with consultation personnel so that they can extend their care to a larger patient population.
Task 5: Full Scale Development and Integration (t = 6-12 months)
This task expands the system to incorporate the greater network and systems of the DoD and civilian workplaces using a defined interoperability standard and reference data standards.
POTENTIAL FUNDING:
The U.S. Government (USG) Department of Defense (DoD) currently has available up to $7 Million (M) FY20 funds for Tasks 1, 2, and 3 of this program. The USG may apply additional dollars for follow-on efforts via post award modification to any resultant awards after the evaluation and acceptance of work and cost plan. Dependent on the results and deliverables, additional time may be added to the period of performance for follow-on tasks.
MTEC expects to make up to six (6) initial awards to qualified teams to accomplish the initial enhanced development effort within the statement of work. However, at each discrete phase of the project, the number of awardees may be down selected based on evaluation factors. If proposed projects are unable to sufficiently address the entire scope of work, several Offerors may be asked to work together in a collaborative manner. See the “MTEC Member Teaming” section below for more details. However, if an optimal team is not identified, then MTEC may make multiple, individual awards to Offeror(s) to accomplish subset(s) of the key tasks.
The anticipated Period of Performance (PoP) for Tasks 1, 2, and 3 is up to 45 days. Dependent on the results and deliverables, additional time may be added to the period of performance for follow-on tasks [e.g., up to 18 months for Tasks 1 – 5].
ACQUISITION APPROACH:
The MTEC will implement the “Enhanced White Paper” contracting methodology for this RPP, which will be an accelerated approach to award. Because of the nature and urgency of the program’s requirements, this streamlined approach is anticipated to be a better means to highlight company methodologies and skills required to address the technical and transition requirements. The Enhanced White Paper process requires extremely quick turnaround times by Offerors. MTEC anticipates that awards will be issued within 6 weeks of the RPP release date. For more information regarding the requirements of the Enhanced White Paper process and template, refer to the RPP.
MTEC MEMBER TEAMING:
While teaming is not required for this effort, Offerors are encouraged to consider teaming during the proposal preparation period (prior to proposal submission) if they cannot address the full scope of technical requirements of the RPP or otherwise believe a team may be beneficial to the Government. MTEC members are encouraged to use the MTEC Database Collaboration Tool to help identify potential teaming partners among other MTEC members. The Database Collaboration Tool provides a quick and easy way to search the membership for specific technology capabilities, collaboration interest, core business areas/focus, R&D highlights/projects, and technical expertise. Contact information for each organization is provided as part of the member profile in the collaboration database tool to foster follow-up conversations between members as needed.
The Collaboration Database Tool can be accessed via the “MTEC Profiles Site” tab on the MTEC members-only website.
MTEC:
The MTEC mission is to assist the U.S. Army Medical Research and Development Command (USAMRDC) by providing cutting-edge technologies and supporting life cycle management to transition medical solutions to industry that protect, treat, and optimize Warfighters’ health and performance across the full spectrum of military operations. MTEC is a biomedical technology consortium collaborating with multiple government agencies under a 10-year renewable Other Transaction Agreement (OTA), Agreement No. W81XWH-15-9-0001, with the U.S. Army Medical Research Acquisition Activity (USAMRAA). MTEC is currently recruiting a broad and diverse membership that includes representatives from large businesses, small businesses, “nontraditional” defense contractors, academic research institutions and not-for-profit organizations.
ADMINISTRATIVE INFORMATION:
Enhanced White Papers are due no later than April 27 at 12:00pm Eastern Time. Due to the critical and urgent nature of the technical topic area, MTEC membership is NOT required for the submission of an Enhanced White Paper in response to this MTEC RPP. However, membership will be required for Offerors recommended for award. For information on how to join MTEC, please visit http://mtec-sc.org/how-to-join/
The full RPP is posted to the MTEC website https://www.mtec-sc.org/solicitations/
POINTS OF CONTACT:
For inquiries regarding this RPP, please direct your correspondence to the following contacts:
- Technical and membership questions – Dr. Lauren Palestrini, MTEC Director of Research, [email protected]
- Programmatic questions – Ms. Kathy Zolman, MTEC Director of Program Operations, [email protected]
- MTEC Member Collaboration Database Tool – Ms. Melissa Sanchez, MTEC Executive Assistant, [email protected]
To view the solicitation, please click here.
